Services
Paediatric Conditions

Our paediatric physiotherapist can provide specialised physiotherapy treatment for children aged between 0 and 18 years that have difficulty with their physical development as a result of neurological and/or developmental problems.
Neurological conditions can be as a result of problems with the brain, spinal cord or peripheral nerves. Babies and/or children with neurological conditions may have difficulties with their physical functions including mobility, muscle strength, range of movement and balance
Physiotherapy treatment for children with neurological or developmental problems will help to maximise their potential and promote physical development to reach specific milestones (e.g. rolling, crawling and walking).
Suzanne has extensive experience in a variety of neurological paediatric conditions including:
- Cerebral palsy, spina bifida
- Developmental disorders including delay and motor learning difficulties (DCD)
- Acquired brain injuries
- Diseases and injuries of the spinal cord e.g. transverse myelitis, SCI
- Peripheral nerve injuries
- Neuromuscular disorders e.g. dystrophies, myopathies
- Orthopaedic conditions e.g. talipes, torticollis/plagiocephaly, limb deficiencies, recovery post fracture
Initial assessment of your child will include their development, movement, strength and balance in order to produce a structured treatment programme which may include:
- Stretching
- Strengthening
- Re-educating normal movement patterns
- Balance training
- Improving standing and quality of walking
- Advice and support for parents and or teachers
- Milestone development
- Working on fine and gross motor skills
The treatment approach will depend on your child's individual circumstances in order to provide the best possible treatment. It can be carried out either at the clinic or in your own home or at their school or nursery, depending on your child's needs. Early intervention is of key importance for your child to maximise their potential and can be provided as soon as possible as there are no waiting lists.
What causes knee pain?

The knee joint is where the thigh and shin bones meet. The end of each bone is covered with cartilage, which allows the ends of the bones to move against each other almost without friction. The knee joint has two extra pieces of cartilage called menisci, which spread the load more evenly across the knee.
The knee joint is held in place by four large ligaments. These are thick, strong bands which run within or just outside the joint capsule. Together with the capsule, the ligaments prevent the bones moving in the wrong directions or dislocating. The thigh muscles (quadriceps) also help to hold the knee joint in place.
Many factors can increase your risk of osteoarthritis of the knee. It’s most common if:
- you’re in your late 40s or older – this might be because your muscles have become weaker, your body is less able to heal itself or your joints have gradually worn out over time
- you’re a woman – osteoarthritis is more common and more severe in women
- you’re overweight – this increases the chances of developing osteoarthritis and of it becoming gradually worse
- your parents or siblings have had osteoarthritis
- you’ve had a knee injury, for example a torn meniscus
- you've had an operation on your knee, for example a meniscectomy (to remove damaged cartilage) or repairs to your cruciate ligaments
- you do a hard, repetitive activity or a physically demanding job, for example farming or mining
- you have another type of joint disease which has damaged your joints, for example rheumatoid arthritis or gout.
What can be done to help?
If your knee pain is affecting your activity and is persisting, ask your GP about referral to a physiotherapist. Physiotherapy can help you to manage pain and improve your strength and flexibility. A physiotherapist can provide a variety of treatments, help you understand your problem and get you back to your normal activities.
| Condition | Common Signs & Symptoms | |||||
| Pain | Swelling | Stiffness | Weakness | Instability | Locking | |
|
ACL Knee Injury & Reconstruction (Anterior Cruciate Ligament Rupture) |
||||||
| Torn Cartilage Knee Injury (Meniscus Tear) |
||||||
| Runner's Knee (IlioTibial Band Friction Syndrome) |
||||||
| LCL Knee Ligament Injury (Scaphoid Fracture) |
||||||
|
MCL Knee Ligament Injury (Medial Collateral Ligament Injury) |
||||||
| Osgood Schlatters (Osgoods) |
||||||
| Knee Arthritis (Osteoarthritis of the Knee) (Knee Arthritis) |
||||||
| Osteochondritis Dissecans (OCD) (Loose Bone Fragments in the Knee Joint) |
||||||
| Patella Fracture (Knee Fracture) (Broken Knee Cap) |
||||||
| Jumpers Knee (Patella Tendonitis) (Patella Tendinopathy) |
||||||
| Patellofemoral Pain Syndrome (Anterior Knee Pain) (Patellafemoral Maltracking) (Chondromalacia Patella) |
||||||
| PCL Tear (Posterior Cruciate Ligament Tear) |
||||||
What causes back pain?

Back pain is common but most cases aren’t caused by a serious problem. Most cases of back pain get better on their own within a few weeks.
Stay active. Bed rest for more than a couple of days makes it harder to get going. Gradually increase your normal activities and do regular exercise.
As well as the factors listed above, there are also specific conditions which are associated with pain felt in the back.
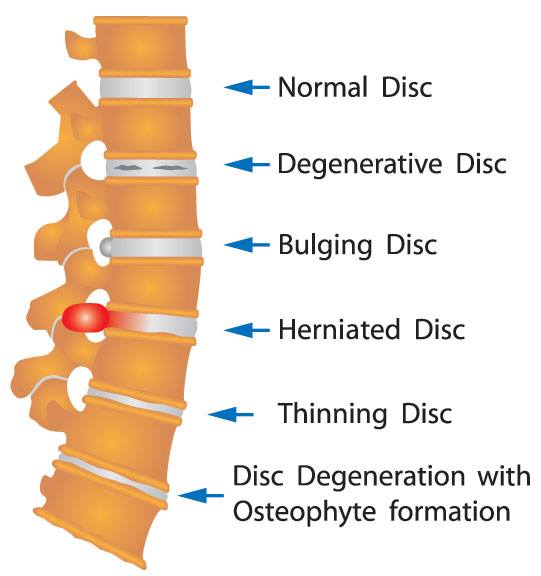
Spondylosis
As we grow older the discs in the spine become thinner and the spaces between the vertebrae become narrower. Spurs of bone (osteophytes) may form at the edges of the vertebrae and facet joints. This is called spondylosis. All of us will have some of these changes in our spine as we get older, but they will not cause all of us pain.
Sciatica
Back pain is sometimes linked with pain in the legs, and there may be numbness or a tingling feeling. This is called sciatica. This is due to irritation or squeezing of one of the spinal nerves (called the sciatic nerve). For most people who develop sciatica, the leg pain tends to be the most troublesome symptom and they may not have back pain at all.
Pain travels down the leg because of the irritation of the sciatic nerve in the lumbar spine, but there’s actually nothing wrong with the leg itself. In most cases the reason for the nerve irritation is a bulging disc. Discs are designed to bulge but sometimes a bulge can 'catch' on the sciatic nerve roots causing pain that travels all down the leg to the foot.
Sciatica is fairly uncommon and fortunately most people recover fairly quickly, although in some cases it might take a number of months. About 60% of all people with sciatica get better within a few weeks to months.
Spinal stenosis
Spinal stenosis is back pain linked with pain in the legs which starts after a few minutes’ walking and tends to get better very quickly when you sit down. This can happen from birth or develop as we get older.
Symptoms often affect both legs but one may be worse than the other. The pain usually eases when you sit down and rest, and some people have less discomfort if they walk a little stooped. Like sciatica, the main problem tends to be leg pain more than back pain.
In most cases, neither sciatica nor spinal stenosis are causes for alarm, but if the symptoms cause you a lot of trouble and greatly affect your quality of life then you should see your doctor for further advice and to discuss what else can be done.
Other rarer causes of back pain include:
- bone problems such as a fracture – often linked to thinning of the bones (osteoporosis)
- an infection
- a tumour
- inflammation, such as in ankylosing spondylitis.
What can be done to help?
Physiotherapy can be useful to improve your strength and flexibility. A physiotherapist can help oversee your exercise programme and recommend specific exercises to help.
Manual therapies (‘hands on’ treatments), such as manipulation and mobilisation of the spinal joints, can help. These techniques are usually carried out by osteopaths, chiropractors and physiotherapists.
| Condition | Common Signs & Symptoms | |||||
| Pain | Swelling | Stiffness | Weakness | Instability | Locking | |
|
Facet Syndrome (Zygoapophyseal Joint Pain) |
||||||
| Herniated Disc (Slipped Disc) |
||||||
| Sacro Iliac Joint Dysfunction (SI Joint Dysfunction) Note: This is classed as a Pelvis Injury |
||||||
| Sciatica | ||||||
| Side Strain (Tear of the Oblique Muscles) |
||||||
| Spinal Stenosis | ||||||
| Spondylolysis (Lower Back Stress Fracture) |
||||||
What causes foot pain?
Most feet have an arch shape that spreads the body's weight evenly over many bones and joints. Feet with lower arches tend to be more flexible, while feet with higher arches are generally less flexible. High or low arches aren’t necessarily a problem but they can increase your chances of developing other foot problems.
The structure of the foot changes as we get older or if arthritis affects the foot joints, and many people will notice changes, particularly in the arch of the foot.
The feet and ankles can be affected by several types of arthritis, including osteoarthritis and inflammatory arthritis.
Osteoarthritis
Osteoarthritis can affect any joint in the foot. Osteoarthritis is a chronic problem that may cause episodic pain and swelling in a joint or joints; it can also cause bone enlargement. As people get older, osteoarthritis can be linked to changes in the shape of feet, which may cause pain.
Osteoarthritis often affects the big toe joint. The joint will become stiffer and the range of movement will be reduced. Often the bones become larger and knobbly due to an overgrowth of new bone. These changes may accompany a bunion (a lump on the side of the big toe joint). You may also notice a bunionette (a lump on the side of the little toe joint).
Recent findings suggest that osteoarthritis is more common in the arch area of the foot than previously thought. Osteoarthritis can also develop in the ankle, but this is usually following a previous injury or damage to the joint from long-standing inflammatory arthritis. Osteoarthritis in the feet often accompanies osteoarthritis in other joints.
Inflammatory arthritis
There are various forms of inflammatory arthritis, which can affect feet in different ways.
- Rheumatoid arthritis can affect many joints in the feet.
- Reactive arthritis usually affects the ankle or the area around the heel. It may also affect the toes, causing pain and swelling, which is known as dactylitis.
- Psoriatic arthritis often causes dactylitis.
- Gout most commonly affects the big toe joint. It is a very painful type of arthritis. Gout causes severe inflammation and makes the joint red, hot and swollen during an attack, which typically lasts one to two weeks. Without treatment, repeated attacks can cause permanent damage to the joint and lead to osteoarthritis. It is caused by the formation of urate crystals in a joint. However, gout can usually be well controlled with medications.
- Ankylosing spondylitis mainly affects the spine but may also affect the heels.
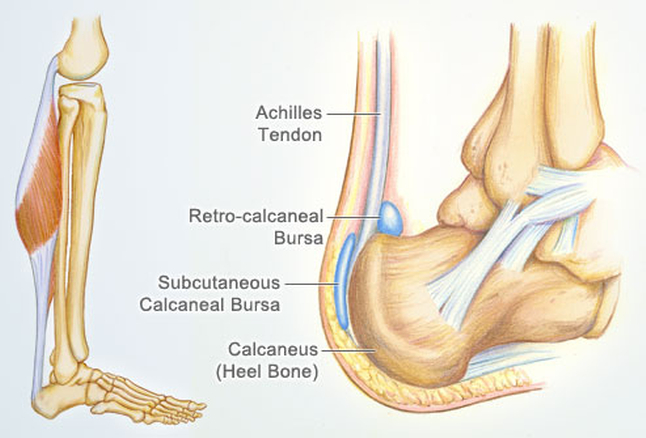
Apart from problems in the joints themselves, people with inflammatory arthritis may have inflammation and discomfort in the tendons and the other soft tissues in the feet. The part under or behind the heel where the tendons attach to the heel bone (the Achilles tendon) is quite often affected in this way.
Connective tissue disease
Raynaud's phenomenon is a circulatory problem that causes the blood supply to certain parts of the body to be reduced, especially when exposed to cold conditions. It more commonly affects fingers, but it can also cause toes to temporarily cold and numb and turn white, then blue, then red. These attacks often only last a few minutes, and moving into a warmer environment often stops the attack. Wearing warm gloves and socks may help to prevent an attack. Raynaud's phenomenon can occur with the conditions:
- rheumatoid arthritis
- scleroderma/li>
- systemic lupus erythematosus (SLE).
Watch out for ulcers on the toes, or a colour change which doesn't go away as quickly as usual. These problems are usually very painful. If you develop one of these symptoms, you should see your doctor or contact your rheumatology nurse specialist as soon as possible.
Sometimes with lupus the joints and tendons are affected and you may notice that the toes drift outwards and the arches may flatten. This can be painful and may cause a feeling of stiffness after periods of rest.
What can be done to help?
Therapeutic massage can help to reduce pain or tiredness in the feet. Massage can be combined with a relaxing warm-water footbath, and both of these are fine as long as you don't have any open wounds or sores on your feet.
| Condition | Common Signs & Symptoms | |||||
| Pain | Swelling | Stiffness | Weakness | Instability | Locking | |
|
Sprained Ankle (Ankle Sprain) (Ankle Instability) (Inversion/Eversion Injury of the Ankle) |
||||||
|
High Ankle Sprain (Syndesmosis Sprain) |
||||||
|
Broken Ankle (Ankle Fracture) |
||||||
|
Lisfranc Joint Injury (Ruptured Tarso-Metatarsal Ligaments) |
||||||
|
Metatarsal Fracture (Broken Foot) |
||||||
|
Os Trigonum Syndrome (Floating bone in back of ankle) |
||||||
|
Plantar Fasciitis (Heel Pain) |
||||||
|
Snowboarder's Ankle (Fracture of the Lateral Process of the Talus Bone) |
||||||
|
Tibialis Posterior Pain (Acquired Flat Foot) |
||||||
What causes shoulder pain?
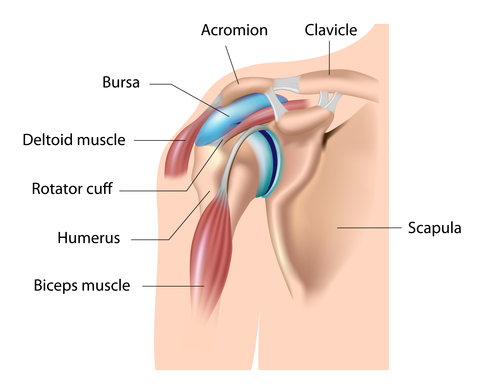
Most shoulder problems will only affect a small area and are fairly short-lived. There are several possible causes, including:
- inflammation or damage to the muscles and tendons around the shoulder
- tension in the muscles between the neck and shoulder (common in people with poor upper back or neck posture, often linked to their work)
- inflammation in the sac of soft tissue (bursa) that normally allows the muscles and tendons to slide smoothly over the shoulder bones
- damage to the bones and cartilage, which can be caused by arthritis.
Referred pain
Shoulder pain isn’t always caused by a problem in your shoulder joint. For example, problems in your neck can cause pain over your shoulder blade or in your upper outer arm. This is known as referred pain.
If you have shoulder pain and a tingling sensation in your arm or hand, this is also more likely to be caused by a problem in your neck.
What can be done to help?
Most shoulder problems will benefit from physiotherapy. A physiotherapist will assess your condition and put together a tailored treatment programme.
The aim of physiotherapy is to improve symptoms and restore function. The approach will depend on whether you have a short-term (acute) problem or a long-standing (chronic) condition. Almost everyone will benefit from a physiotherapy programme, which might include:
- exercises to strengthen weakened muscles, change their co-ordination and improve function
- advice on improving shoulder, neck and spine posture
- exercises to ease or prevent stiffness
- exercises to increase the range of joint movement
- applying adhesive tape to the skin to reduce the strain on the tissues and to help increase your awareness of the position of the shoulder and shoulder blade
- manual treatments to the soft tissues and joints.
| Condition | Common Signs & Symptoms | |||||
| Pain | Swelling | Stiffness | Weakness | Instability | Locking | |
|
Broken Collar Bone (Broken Clavicle) |
||||||
|
Dislocated Shoulder (Shoulder Dislocation) |
||||||
|
Frozen Shoulder (Adhesive Capsulitis) |
||||||
|
Rotator Cuff Calcific Tendonitis (Calcific Tendinopathy) |
||||||
|
Rotator Cuff Injury (Shoulder Tendonitis) (Supraspinatus Tendonitis) |
||||||
|
Shoulder Bursitis (Shoulder Impingement Syndrome) (Subacromial Bursitis) |
||||||
|
Shoulder Separation (AC Joint Sprain) (Acromioclavicluar Joint Sprain) |
||||||
What causes neck pain?
Pain and stiffness
You may feel pain in the middle or on either side of you neck, but it may also extend to the shoulder and shoulder blade, or to the upper chest.
If you have tension headaches, the pain often travels to the back of your head, and sometimes behind your eye or even into your ear.
It may be painful to move and your muscles may feel tight, especially if you've been sitting in one position for a long time. You may notice your neck doesn't turn as far as it normally does, for example when you try to look over your shoulder while reversing the car.
If your neck stiffness came on quickly, you are aged 50 or over. and you also have stiffness in both shoulders that isn't related to a recent injury, this can be a sign of a condition called polymyalgia rheumatica (PMR) – an inflammatory condition affecting the muscles. You should see your doctor as soon as possible as this condition needs to be treated promptly.
Numbness or tingling
If a nerve root is being pinched you may have numbness, tingling or pins and needles down your arm, sometimes right down to the fingers.
Clicking and grating noises
You may hear or feel clicking or grating as you move your head – this is called crepitus, and is caused by bony surfaces moving against each other or by ligaments moving over bone. Other joints often do this too but noises from your neck usually seem louder because they're happening closer to your ears. You may also find they're more noticeable at night. This is quite common and can sound alarming but it's not serious.
Dizziness and blackouts
If you feel dizzy when looking up or turning your head, this may be caused by the vertebral arteries being pinched. This sometimes happens as a result of changes in the bones of the spine. Pinching of these arteries can sometimes cause blackouts as the blood flow is temporarily reduced. However, this kind of dizziness can have other causes (for example, problems in the ear) so it's best to see your doctor if the problem continues.
Muscle spasms
Sometimes if you have neck pain you may also have muscle spasms that turn your head to one side. This is called torticollis, cervical dystonia or acute wry neck. This isn't very common but is unpleasant. The problem usually only lasts a few hours or days, but rarely may continue for several weeks.
Other symptoms
If you have long-lasting neck pain, and especially if your sleep is disturbed, then you may feel extremely tired and, not surprisingly, rather down or low in mood. You should speak to your doctor, family and friends if neck pain is getting you down.
What can be done to help?
Physiotherapists, chiropractors and osteopaths are all trained to treat neck problems. Treatment carried out by one of these therapists, along with home exercises, are often all that’s needed. It’s important to make sure that any physical treatments are given by qualified practitioners.
Manipulation
Manipulation is a type of manual therapy used to adjust parts of your body to treat stiffness. It can sometimes be uncomfortable at the time, so it's important to understand what’s involved. Talk to your therapist about the treatments before they start. Your therapist should ask you about osteoporosis, as some treatments aren’t suitable for people with this condition. Recent research suggests that manipulation usually works best within the first three months of developing a neck problem.
The Alexander Technique
The Alexander Technique is a method of teaching bodily awareness and reducing unwanted muscle tension. A qualified teacher will advise you on your sitting and standing posture and your patterns of movement. Some physiotherapists are trained in this technique but it's not always available on the NHS.
TENS (transcutaneous electrical nerve stimulation)
A TENS machine is a small battery-driven machine which may help to reduce pain in the short term. Small pads are placed over the painful area and low-voltage electrical stimulation produces a pleasant tingling sensation. It's suggested that this can interfere with pain signals from the nerves to the brain. You can buy TENS machines from pharmacies, but your physiotherapist may be able to let you borrow one to try first.
Collars
Some people find a special collar helpful if a pinched nerve is causing pain that can be felt down the arm. However, there's little research evidence that they help with either short-term or long-term neck pain. The use of collars for neck problems varies across the UK – some healthcare professionals suggest they promote stiffness whereas others believe they can be helpful as long as they're fitted well and not used for long periods of time.
| Condition | Common Signs & Symptoms | |||||
| Pain | Swelling | Stiffness | Weakness | Instability | Locking | |
|
Broken Neck (Cervical Fracture) |
||||||
|
Slipped Disc in Neck (Cervical Disc Prolapse) |
||||||
|
Stiff Neck (Wry Neck) (Acute Torticollis) |
||||||
|
Whiplash (Whiplash Associated Disorder - WAD) |
||||||
What causes Hand and Wrist pain?
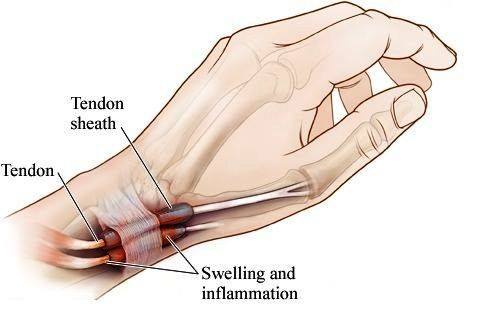
When the nerve is squeezed it can cause pain, aching, tingling or numbness in the affected hand. The symptoms tend to be worse at night and may disturb your sleep, but you may notice it most when you wake up in the morning. Hanging your hand out of bed or shaking it around will often relieve the pain and tingling.
You may not notice the problem at all during the day, though certain activities – such as writing, typing, DIY or housework – can bring on symptoms.
Sometimes the condition can be mistaken for something else. For example, pressure on nerves in the neck due to disc problems or arthritis can cause similar symptoms.
A nerve conduction test may help if there’s any doubt about the diagnosis.
What causes carpal tunnel syndrome?
Carpal tunnel syndrome is a common problem. It’s often caused by work-related activities, such as typing, and repetitive movements, although some cases may be related to arthritis of the wrist, thyroid disease and pregnancy. Your risk of developing it may be greater if your job places heavy demands on your wrist or if you use vibrating tools.
What can be done to help?
If there’s a particular cause, like an underactive thyroid or arthritis, treating that condition may help. Other treatment will depend on how severe the nerve compression is. It’s important to get help quickly if your hand muscles are weak.
| Condition | Common Signs & Symptoms | |||||
| Pain | Swelling | Stiffness | Weakness | Instability | Locking | |
|
Bennett's Fracture (Fracture Dislocation of the Thumb) |
||||||
| Broken Wrist (Capitate Fracture) |
||||||
| Broken Wrist (Colles Fracture) |
||||||
| Broken Wrist (Scaphoid Fracture) |
||||||
| Carpal Tunnel Syndrome | ||||||
| Mallet Finger (Baseball Finger) |
||||||
| Sprained Thumb (Skier's Thumb) |
||||||
| Wrist Arthritis (Osteoarthritis of the Wrist) |
||||||
What causes hip pain?
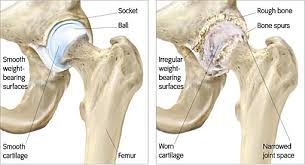
Most hip pain has a very simple explanation, for example if you’ve overdone it while exercising. The pain is usually caused by strained or inflamed soft tissues such as tendons, and it often clears up within a few days. Long-term hip pain can be caused by specific conditions.
Pain caused by a problem in the hip joint can be felt in the groin, down the front of the leg and in the knee. Sometimes knee pain is the only sign of a hip problem. This is called referred pain, and it’s fairly common. Hip pain can also be felt in the buttock (although pain in this area can also be caused by problems with the lower back) or on the outside of the hip.
What can be done to help?
Physiotherapy may help you to maintain your hip movements with gentle range of movement exercises and activities.
A physiotherapist can also suggest specific exercises to maintain or improve the strength of the muscles around the hip joint. They may advise you about the best way to walk with your hip pain and may help you to use a stick or crutch.
You’ll need to use the stick in the opposite hand to your affected hip and make sure that it’s the correct height for you, so it’s important to see a physiotherapist before you start using one.
| Condition | Common Signs & Symptoms | |||||
| Pain | Swelling | Stiffness | Weakness | Instability | Locking | |
|
Hamstring Injury (Hamstring Muscle Strain) (Pulled Hamstring) |
||||||
|
Hip Arthritis (Osteoarthritis of the Hip) |
||||||
|
Hip Bursitis (Trochanteric Bursitis) |
||||||
|
Hip Labrum Tear (Acetabular Labrum Tear) |
||||||
| Thigh Muscle Strain | ||||||
Women’s Health
This concerns physical problems related to pregnancy and gynaecological associated conditions. There are other physical discomforts not directly related to pregnancy that women are affected by, which can be helped by physiotherapy. We also offer a range of services for women during pregnancy such as appropriate exercise.
From incontinence to prolapse, pelvic pain or constipation, there is growing evidence that physiotherapy can alleviate, and in many cases cure these symptoms. Most women don’t know that help is available and it can be an embarrassing topic so I hope that these pages are helpful in answering some of the questions you may have about your body and whether Women’s Health Physiotherapy can help you.
- How can Women’s Health Physiotherapy help my pelvic floor?
- How can Women’s Health Physiotherapy help me during pregnancy?
- How can Women’s Health Physiotherapy help me post-natally?
- What can I expect at my Women’s Health Physiotherapy appointment?
How can Women’s Health Physiotherapy help my pelvic floor?
The pelvic floor is a complex structure made up of a group of muscles that support the pelvic organs and form the the birth canal and passages for urine and stool.
The pelvic floor muscles are often described as a hammock lifting and supporting the pelvic organs above.
These muscles need to be able to contract to keep us continent, but also they must relax to allow for urination, bowel movements, child birth and sexual intercourse.
Problems with the pelvic floor can occur when these muscles are too weak (hypotonic) or too tight (hypertonic). It is also possible for these muscles to combine a pattern of too much tension in some areas while too relaxed in others!
When the pelvic floor muscles are low- tone (hypotonic) the hammock becomes less effective at supporting the pelvic organs and symptoms such as urinary or bowel incontinence, urgency and pelvic organ prolapse can occur. These are NOT a normal part of aging and the muscles can become weak for many reasons.
The good news is that a structured exercise program to strengthen the pelvic floor muscles is effective in reversing the symptoms in 80% of women.
Following an assessment treatments for the symptoms of hypotonic pelvic floor muscles include:
- Pelvic floor re-training and exercises
- Provision of pelvic floor educators/muscle stimulators to improve your activation and power of your pelvic floor contraction
- Pilates based pelvic stability exercises to strengthen the abdominal muscles which play a supporting role in the strength of the pelvic floor
- Assessment and treatment of any low back/pelvic pain issues which can lead to weakness of the pelvic floor muscles
When the pelvic floor muscles are high-tone (Hypertonic) they can cause urinary frequency, urgency, hesitancy or incomplete emptying and painful urination as the muscles are unable to relax fully to allow the passage of urine down the urethra. You may also experience constipation or pain with bowel movements, unexplained pain in your low back, pelvic region or genital area, pain during or after intercourse, orgasm, or sexual stimulation due to the tension in these muscles.
Hypertonic pelvic floor muscles can also contribute to Interstitial Cystitis, Vulvodynia and Pudendal nerve Neuralgia. There are again many reasons for these changes to occur in the pelvic floor muscles but hypertonicity may follow trauma to the pelvic floor/pelvic organs (for example in childbirth), following gynaecological intervention or investigation, unresolved low back or hip pain or following an infection.
When the pelvic floor muscles are already in a state of increased tone you may find it difficult to initiate or hold a pelvic floor contraction and increase the tone any further. In this case it is important to relax the pelvic floor muscles fully and treat the tension before any underlying weakness. Once the muscles have reached a normal resting tone, and are able to relax fully, their strength is reassessed and strengthening exercises are prescribed. Following an assessment treatment for the symptoms of hypertonic pelvic floor may include:
- Internal manual therapy techniques to relax the pelvic floor muscles, including trigger point release, myofascial stretches, scar massage,
- neural mobilisations
- Myo-fascial release of the connective tissue of the abdomen, hips and pelvis which support the pelvic floor
- Relaxation and breathing techniques
- Advice on toileting and positional modifications
- Provision of pelvic floor exercises and general exercise to assist in release and re-training of the pelvic muscles
- Provision of vaginal dilators, pelvic floor educators or muscle stimulators to assist in the release and relaxation of pelvic muscles
- Assessment and treatment of any unresolved low back, hip or pelvic pain
- As and when suitable pelvic floor muscle strengthening can begin
If an internal examination is too painful, the connective tissue of your abdomen, thighs, groins and low back can often be very tight. The connective tissue forms the container of the muscles, and this tissue often needs to be relaxed before any internal work can be done. Understanding how our pain systems work has been shown to be an effective way of reducing the threat of on-going pelvic floor dysfunction. Anxiety, stress, thoughts, attitudes and beliefs can perpetuate pain in the pelvis; education about persistent pain is an important part of treating pelvic floor dysfunction since the pelvic area is an area that we often hold our stress.
How can Women’s Health Physiotherapy help me during pregnancy?
Pelvic girdle pain and stress urinary incontinence are common amongst pregnant women. These symptoms often occur due to hormonal changes and the ever increasing weight of your baby and uterus.
The mounting pressure of the uterus on your bladder gives you less room to store urine just when it’s becoming more difficult to stop the flow. You may notice that you leak urine when you sneeze or find it harder to hold your urine when you need to ‘go’. Urinary incontinence in pregnancy should not be ignored as research suggests that if you develop stress urinary incontinence during your pregnancy, or within 6 weeks following the birth of your baby, you are more likely to suffer from incontinence 5 years later.
An assessment with a Women’s Health Physiotherapist is often all you need to prevent this. Making sure that you are doing the right pelvic floor exercises; activating the correct muscles for a suitable length of time is important in maintaining a strong pelvic floor through your pregnancy and beyond.
Pilates based pelvic stability exercises are also valuable through pregnancy to strengthen the supporting muscles of the pelvis and ease the pressure on the pelvic floor. An internal assessment may not be appropriate whilst you are pregnant and therefore an assessment of the muscles of your abdomen and pelvis is often an efficient way of pelvic floor re-training in pregnancy.
1 in 3 women experience low back pain during pregnancy whilst 1 in 5 experience pelvic girdle pain. This is often a result of the hormones Relaxin and Oestrogen relaxing the ligaments which support your pelvis. Your pelvis bones and sacrum slot together like a loose puzzle relying on the ligaments and muscles to provide joint stability. In pregnancy the extra strain on these ligaments can cause pain and movement dysfunction. In such conditions the muscles supporting these ligaments become extra important in providing stability and control. There is much evidence to support physiotherapy for pelvic pain in pregnancy and the treatments you may be offered include:
- Manual therapy techniques
- Connective tissue release of the abdomen, back, hips and pelvis
- Provision of Pilates based pelvic stability exercises
- Acupuncture
- Provision and fitting of pelvic stability belts
- Advice on sleeping positions, exercise and movement modification
How can Women’s Health Physiotherapy help me postnatally?
The immediate weeks after the birth of your baby is an important time for your body. Your body undergoes many changes during pregnancy and continues to change post-natally. It is important to address any issues that occur at this time so as to prevent problems later in life. Childbirth can lead to pelvic floor trauma, perineal tears and pudendal nerve injury (the nerve which supplies your bladder and pelvic floor). Consequently the pelvic floor can become dysfunctional and you may experience urinary or bowel urgency and/or incontinence, urinary frequency, incomplete emptying, pain on urination/defeacation and pain or discomfort with sexual intercourse.
A pelvic floor assessment is important to establish the cause of these symptoms.
A Women’s Health Physiotherapist can assess you from 6 weeks post-natally or after your 6-week check up.
Following your assessment appropriate treatment can be provided which may include:
- Pelvic floor re-training and exercises
- Provision of pelvic floor educators/muscle stimulators to improve your activation and power of your pelvic floor contraction
- Internal manual therapy techniques to relax the pelvic floor muscles, including trigger point release, myo-fascial stretches, scar massage, neural mobilisations.
- Myo-fascial release of the connective tissue of the abdomen, hips and pelvis which support the pelvic floor
- Relaxation and breathing techniques
- Advice on toileting and positional modifications
- Provision of pelvic floor exercises and general exercise to assist in release and re-training of the pelvic muscles
- Provision of vaginal dilators, pelvic floor educators or muscle stimulators to assist in the release and relaxation of pelvic muscles
- Assessment and treatment of any unresolved low back, hip or pelvic pain
A Women’s Health Physiotherapist can also help with advice on return to exercise and healing of separated abdominal muscles (Diastasis Recti). Diastasis Recti often occurs in the third trimester of pregnancy when the abdominal muscles are at their greatest stretch. The linea alba normally joins the left and right hand rectus abdominal muscles. When the linea alba is overstretched a separation can occur between the left and right sides. Diastasis recti may make it harder for you to regain your tummy tone and return to your normal exercise routine. It is important to have an assessment to determine if your muscles are stretched; “Divarification Recti” or separated “Diastasis Recti” as this will determine which exercises are suitable for you. An assessment can be carried out from 6 weeks if you had a vaginal delivery or 8 weeks if you had a C-section.
What can I expect at my first Women’s Health Physiotherapy appointment?
Your assessment and treatment will depend upon your presenting condition. We will start with taking a confidential and detailed history. Whilst these sensitive issues are often difficult to discuss, understanding the onset of your symptoms and how your daily life is affected is vital in directing your treatment. Your physical assessment will most likely begin with examination of your abdominal muscles, pelvis and lumbar spineFollowing this assessment you may be offered an internal examination. This is an important part of your examination and necessary in identifying the tone, strength and control of your pelvic floor muscles. Using finger palpation the pelvic floor muscles and connective tissue will be assessed for injury or scarring, signs of pelvic organ prolapse, muscle tone, tenderness, sensation and neural sensitivity. Following this the pelvic floor muscle will be tested for strength and endurance. It is important to determine if the left and right, superficial and deep pelvic floor muscles are working together, and if not why not. Once we establish your baseline of pelvic floor muscle control we can then develop a specific and individualised exercise programme. The assessment findings will be discussed with you and treatment will depend upon findings and your symptoms.
What causes of Myofascial Pain

Myofascial pain can have two sources. Pain can be generated from the skeletal muscle or connective tissues that are 'bound down' by tight fascia. In addition, pain can also be generated from damaged myofascial tissue itself, sometimes at a 'trigger point' where a contraction of muscle fibers has occurred. In either case, the restriction or contraction inhibits blood flow to the affected structures, thus accentuating the contraction process further unless the area is treated.
Myofascial Release Therapy
Myofascial release (MFR) therapy focuses on releasing muscular shortness and tightness. There are a number of conditions and symptoms that myofascial release therapy addresses.
Many patients seek myofascial treatment after losing flexibility or function following an injury or if experiencing ongoing back, shoulder, hip, or virtually pain in any area containing soft tissue.
Other conditions treated by myofascial release therapy include Temporo-Mandibular Joint (TMJ) disorder, carpal tunnel syndrome, or possibly fibromyalgia or migraine headaches. Patient symptoms usually include:
- Tightness of the tissues that restricts motion or pulls the body out of alignment, causing individuals to favor and overuse one hip or shoulder, for example
- A sense of excessive pressure on muscles or joints that produces pain
- Pain in any part or parts of the body, including headache or back pain.
What causes polymyositis and dermatomyositis?

Polymyositis and dermatomyositis are autoimmune diseases where your immune system, which normally protects your body against infections, attacks your body’s own tissues. This causes inflammation in your muscles and skin.
Polymyositis and dermatomyositis are rare diseases, affecting only 6–8 people out of 100,000. They mostly affect adults, although children can be affected by a type of dermatomyositis (juvenile dermatomyositis).
symptoms of polymyositis and dermatomyositis?
Most people will only have mild and short-lived symptoms. These can include:
- Weak and tired muscles – making normally easy tasks very tiring
- Inflamed muscles – causing pain (known as myalgia) and feeling tender to the touch
- Generally feeling unwell (malaise)
- Weight loss
- Night sweats
If you have dermatomyositis, you may get some of the above symptoms as well as:
- a red/pink rash on your upper eyelids, face and neck, and on the backs of your hands and fingers
- swelling of the affected skin, causing a characteristic puffiness and colouring around your eyes.
Other conditions can sometimes mimic polymyositis. These include:
- side-effects of some medications (for example, steroids or statins)
- toxic effects of long-term alcohol excess
- hormonal conditions such as under- or over-active thyroid
- low vitamin D levels or abnormal calcium or magnesium levels
- infections
- rarer nerve–muscle diseases such as muscular dystrophies.